Vitamin D
We are emerging from another long and grey Winter. Pale and pallid we crave sunlight. It is well known now that due to the low sunshine levels in the Northern hemisphere and particularly the UK, Vitamin D deficiency is very common. Government recommendations are coming through that all children should take a supplement daily and most adults for at least 3 months of the year.
Vitamin D is vital for a wide variety of bodily functions but most specifically nerve, bone and joint health. It is also linked to mood disorder. An unbalanced approach to skin cancers has also meant that sunblocks further prevent its absorption. Though it is available through some foods, Vitamin D is manufactured in the body through exposure to sunlight.
Studies have shown that low Vitamin D levels can:
- weaken your immune system
- increase the risk of rheumatoid arthritis
- increase the severity of arthritis
- increase the risk of falls for older people
- increase the risk of stress fractures
- cause reduced limb muscle strength
- cause joint pain and aching, particularly with movement
Most people have heard of rickets and will think of Dickensian times and children with deformed and bowed legs. This can be caused by an extreme lack of Vitamin D. But Vitamin D deficiency is on the rise today and risks the health of many adults who are unaware of their own low levels.
Vitamin D helps to control the amount of calcium and phosphate in our bodies, which are needed for healthy bones, teeth and muscles. It is found naturally in only a small number of foods, including oily fish, red meat, liver and egg yolks, as well as fortified breakfast cereals.
Even if you do eat plenty of these foods, it can still be difficult to get the recommended amounts of Vitamin D as the main source is the action of sunlight on our skin.
Vitamin D is often called the sunshine vitamin because your body produces it when skin is exposed to sunlight. Where possible, going outside and exposing your arms and face to sunlight is the best way to get vitamin D. From June to August 15 minutes a day is generally enough. Dark skin needs more exposure, and more exposure is also needed in winter.
We are bombarded with advice about skin cancer awareness, practising ‘safe sun’ and protecting delicate young and older skin from the risks of ageing, so many of us shield ourselves from the sun wherever possible, slapping on copious amounts of sunscreen. But, as with so many things, getting the balance right is important.
Because of the lack of sunlight, slight deficiency is quite common in winter in the UK, especially in the north. There is some evidence that arthritis progresses more quickly in people who don’t have enough vitamin D.
In 2016, in light of this increasing problem, the government’s Scientific Advisory Commission on Nutrition reviewed previous advice and now recommend that all children and adults consider taking a vitamin D supplement, and seeking advice and possibly a test from your GP.
Further studies are under way, looking at the link between low vitamin D and various diseases. So check out your levels and be good to your bones as part of your new commitment to health. They have to hold you up for a lifetime.
Protocol for Vitamin D Treatment
Whenever a vitamin D level of less than 50 nmol/L is discovered there should be a review of the patient’s past medical history including drug history. The BMI should be measured as well as checking renal function (including urinalysis for nephrotic syndrome), calcium and phosphate, liver function, thyroid function, full blood count, ferritin, ESR and CRP. The medical history should consider the possibility of autoimmune disease as well as malabsorption and if appropriate tests for these conditions should be undertaken as well. A PTH level should be considered according to calcium levels.
Treatment should be Colecalciferol (vitamin D3) unless the patient is a vegan when Ergocalciferol (vitamin D2) can be used. Vitamin D3 is available as Fultium-D3 capsules at either 800, 3,200 or 20,000 IU (N.B. excipients include peanut oil). Vitamin D2 is available as either 10,000 or 50,000 IU tablets.
If the vitamin D level is less than 30 than a fixed loading dose of 300,000 IU over 6 – 10 weeks should be prescribed. Schedules may be according to patient preference as daily 4,000 IU for ten weeks, once weekly 50,000 IU for six weeks, or twice weekly 20,000 IU for seven weeks. This should be followed by 1,000 IU daily for life although this should be discontinued if the patient is breastfeeding.
If the vitamin D level is 30 – 50 nmol/L then the dose is 1,000 IU daily for life without a loading dose.
The management in chronic renal failure or severe liver disease or in the presence of an elevated parathyroid hormone should be with specialist assistance.
The parathyroid hormone should be checked six months after starting treatment.
The dietary calcium intake should be calculated and addressed by diet using the calculator available at www.cgem.ed.ac.uk/research/rheumatological/calcium-calculator. If dietary change is not possible then a supplement should be given but this should not be Calcichew D3.
All residents in the UK are currently advised to take a vitamin D supplement of 400 IU daily.
Other News Articles You May Be Interested In
5 Lessons from the UK's Leading Expert in Back Pain
In the world of back pain, Nick Potter is the leading expert in the UK. With clients like Elton John...
A pain in the neck
Do you get neck pain which particularly manifests in the tops of your shoulders, relieved but only temporarily by massage?...
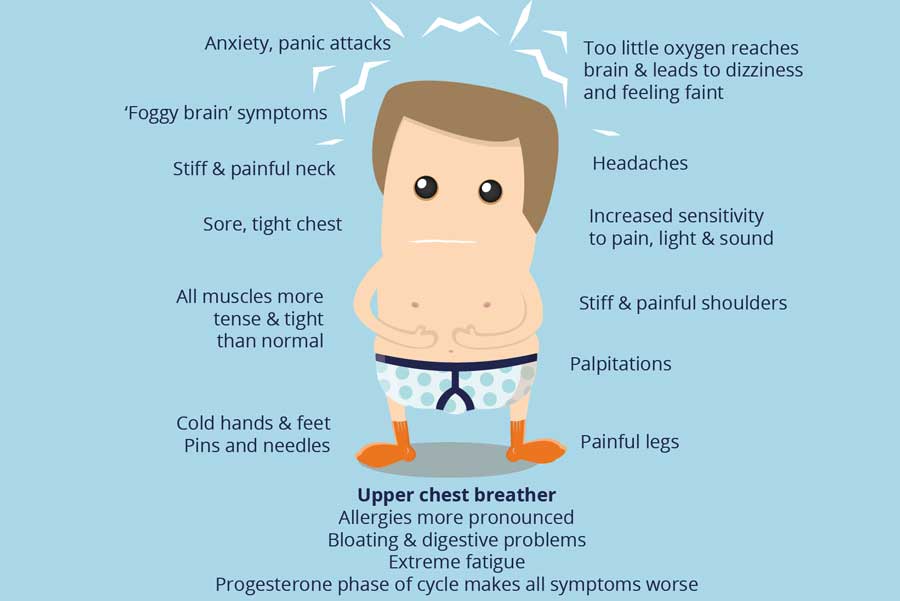
BREATHING, ANXIETY & LUNG HEALTH
BREATHINGWe need to start a breathing revolution. You are about to start something which could and most probably will, change...